CMS Offers Written Guidance on Telehealth Coding and Procedures. Advis Offers Simple Overview of ‘What Providers Need To Know’ to Stay in Compliance
Advis has been at the forefront of regulatory updates surrounding the CMS telehealth waivers related to the COVID-19 update. Although CMS released valuable guidance for telehealth services in the previous weeks, which Advis has summarized in a previous article, many questions remained unanswered. Advis received specific written guidance from CMS addressing the following questions:
1. Question: Are providers allowed to use any CPT/HCPCS codes with place of service (POS) code “02 – telehealth”, or are they restricted to the Medicare Telehealth Codes List?
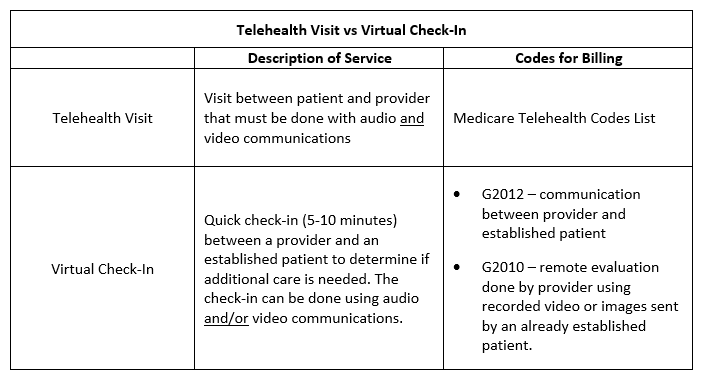
Answer: Providers may only bill for telehealth services using the Medicare Telehealth Codes List. The important change from the waivers is that providers may furnish telehealth services regardless of the Medicare beneficiary’s location.
2. Question: Do the waivers permit the use of audio-only communication to provide telehealth services?
Answer: Providers are required to use devices that are capable of interactive audio and visual communications for telehealth services. However, providers are allowed to use audio and/or video communications for virtual check-in services provided to established patients.
3. Question: Does POS 02 need to be used with virtual check-ins or e-visits (communication between provider and established patient via online portal)?
Answer: No. POS 02 is for telehealth visits only. Visits are distinct from virtual check-ins and e-visits. Providers should use the POS code appropriate for the distant site, e.g., the location of the provider, for virtual check-ins and e-visits.
Please contact any of our COVID-19 task force members with your telehealth questions.
Published: March 27, 2020




