CY2021 MPFS Update: Evaluation, Management & wRVU Changes Potentially Increase PSA Costs
The CY2021 Medicare Physician Fee Schedule (“MPFS”) rule finalized the changes to the wRVU calculations for several services. These changes include significant increases for E/M visit codes. They may also result in increased provider compensation costs for certain entities, such as health systems and hospitals, that utilize wRVU-based provider services agreements.
The wRVU updates were altered the definitions of E/M codes causing them to be more focused on time-based assessments in keeping with recommendations from the AMA RUC and the removal of CPT 99201. The increase in wRVUs is tied to the increase in total time that must be spent with the patient in order to meet the CPT code definitions.
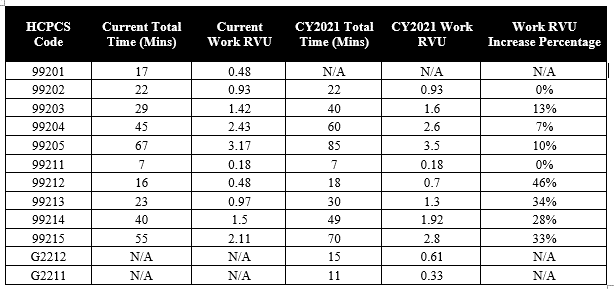
The chart below demonstrates the increase in required physician time as well as the corresponding wRVU increase. The rule also added and clarified language for two new add-on codes G2212 (each additional 15 minutes beyond 99205 or 99215 by the physician or qualified healthcare professional, with or without direct patient contact) and G2211 (serious condition or a complex condition).
CMS also sought to provide increased wRVUs for physicians providing charges analogous to E/M codes in certain specialties. As a result, the following specialties will also experience increased wRVU rates:
- End-Stage Renal Disease (ESRD) Monthly Capitation Payment (MCP) Services;
- Transitional Care Management (TCM) Services;
- Maternity Services;
- Cognitive Impairment Assessment and Care Planning;
- Initial Preventive Physical Examination (IPPE) and Initial and Subsequent Annual Wellness Visits (AWV);
- Emergency Department Visits;
- Therapy Evaluations; and
- Psychiatric Diagnostic Evaluations and Psychotherapy
As a result of the change in E/M and analogous codes, CMS also updated the CY 2021 PFS conversion factor to $32.41, a decrease of $3.68 from the CY2020 PFS conversion factor of $36.09. This reduction was done to ensure a net zero change in rates, in keeping with budget neutrality requirements.
Reach out to Advis today to discuss the potential impact on your facility. Advis can use your existing data to identify a physician payment differential based upon the updated wRVUs from the CY2021 MPFS final rule.
Published: December 4, 2020