In addition to the release of the CY 2021 Outpatient Prospective Payment System (“OPPS”) Proposed Rule, CMS also released the CY 2021 Medicare Physician Fee Schedule (“MPFS”) Proposed Rule. The CY 2021 MPFS Proposed Rule details policy, payment, and quality changes. CMS is accepting public comments until October 5, 2020. A summary of key details within the CY 2021 MPFS Proposed Rule follow below.
1. Physician Rate Setting and Fee Schedule Conversion Factor Payment Update:
CMS has proposed various technical updates and standard rate setting refinements for CY 2021. In addition, CMS has proposed a MPFS conversion factor of $32.26 (the number by which Medicare’s relative value units (“RVUs”) are multiplied to determine payment rates) for 2021, as opposed to a rate of $36.09 in 2020. This reduction is in response to budget neutrality adjustments required by law.
2. Medicare Telehealth Services / Services Involving Communications Technology:
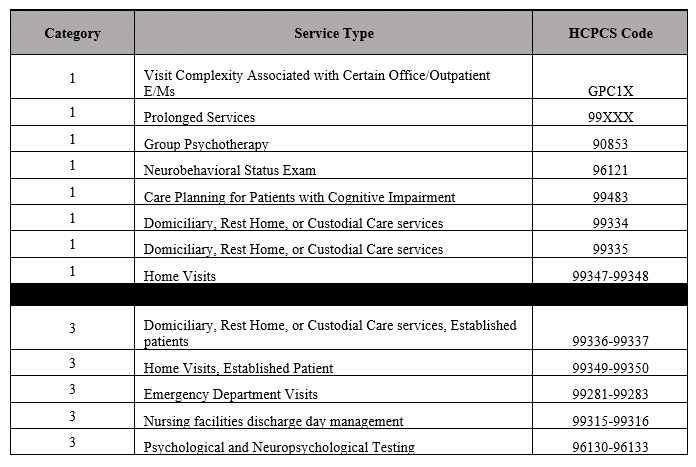
The services below and their corresponding HCPCS Codes have been proposed to be added to the Medicare telehealth list under, respectively, Category 1 and Category 3 designations. The Category 1 services are similar to those already on the telehealth list, whereas the Category 3 services belong to a temporary category that will remain through the calendar year in which the current public health emergency for COVID-19 subsides.
Other CMS comments/proposals include:
-
- Proposed to revise the frequency limitation for subsequent nursing facility visits furnished by Medicare telehealth from one visit every 30 days to one visit every three days;
- Clarified that licensed clinical social workers, clinical psychologists, physical therapists, occupational therapists, and speech-language pathologists can furnish brief online assessment and management services as well as virtual check-ins and remote evaluation services;
- Reiterated that telehealth rules do not apply when the beneficiary and practitioner are in the same location, even if audio/video technology assists in furnishing a service; and
- Although CMS did not propose to continue recognizing payment for audio-only telephone evaluation and management services in the absence of the public health emergency, CMS recognizes that the need for audio-only interactions could remain. Therefore, CMS is seeking comment on whether it should develop coding and payment for a service similar to the virtual check-in, but for a longer unit of time (and higher value).
3. Direct Supervision Definition Update:
CMS previously adopted an interim final policy revising the definition of direct supervision to include virtual presence of the supervising physician or practitioner using interactive audio/visual real-time communications technology. CMS has proposed to allow direct supervision to be provided using real-time audio and video technology (excluding telephone that does not also include video) through December 31, 2021.
CMS is seeking comment from stakeholders regarding the extension of remote direct supervision beyond December 31, 2020, and is also requesting comment regarding potential fraud, abuse, waste, patient privacy, and clinical appropriateness.
4. Payment for Office/Outpatient Evaluation and Management (“E/M”) and Analogous Visits:
The CY 2020 MPFS Final Rule included a plan to align CMS E/M coding and documentation policies with changes by the CPT Editorial Panel for office/outpatient E/M visits, beginning January 1, 2021. CMS has proposed a refinement to clarify the times for when prolonged office/outpatient E/M visits may be reported. CMS has also proposed to revalue various code sets that include, rely upon, or are analogous to office/outpatient E/M visits.
5. Professional Scope of Practice and Related Proposals:
-
- Following the public health emergency, a proposal to make permanent the policy allowing nurse practitioners, clinical nurse specialists, physician assistants, and certified nurse-midwives to supervise, in addition to physicians, the performance of diagnostic tests.
- Reiteration that pharmacists fall within the regulatory definition of auxiliary personnel under “incident to” regulations. Therefore, pharmacists may provide services under the appropriate supervision incident to the services of the billing physician or non-physician practitioner, if payment for the services is not made under Medicare Part D.
- Proposal to make permanent the Part B policy for maintenance therapy services previously adopted on an interim basis for the public health emergency. This allows physical therapists and occupational therapists the discretion to delegate the performance of maintenance therapy services, as clinically appropriate, to a therapy assistant.
- Clarification that physicians and non-physician practitioners, including therapists, can review and verify documentation entered into the medical record by members of the medical team for their own services that are paid under the MPFS. In addition, students working under a physician or practitioner who furnishes and bills directly for their professional services to Medicare, may document in the record so long as it is reviewed and verified by the billing physician or practitioner.
- CMS is considering whether various policies adopted during the public health emergency related to teaching physicians should be extended on a temporary basis or be made permanent.
6. Medicare Shared Savings Program:
CMS has proposed changes to the Medicare Shared Savings Program quality performance standard and reporting requirements for performance years beginning January 1, 2021. For performance year 2020, CMS has proposed to provide automatic full credit for CAHPS patient experience of care surveys. CMS has requested stakeholder comment regarding an alternate scoring methodology to account for the public health emergency from COVID-19 in 2020.
For any questions regarding the Medicare Physician Fee Schedule Proposed Rule, the potential impact on providers, or any other health care regulatory and/or operational matters, please contact Advis or call 708.478.7030.
Published: August 6, 2020





