According to the Center for Medicare & Medicaid Services (CMS), the quality and cost of care for Hip and Knee replacements vary significantly across providers, and at times driving ten miles can mean paying half the price for the same procedure. On average, Medicare expenditure for replacement surgery, hospitalization, and recovery ranges from $16,500 to $33,000.
This large variance in cost reflects an inconsistency in the quality of care and the attention given to reduce post-surgery complications such as infections, readmission, or unnecessarily prolonged recovery periods. As reported by CMS, the hospitalization for these inpatient primary procedures cost more than $7 billion dollars each year.
In an effort to mitigate this national price discrepancy, on July 14th Medicare released changes to the payment system. The proposed Comprehensive Care for Joint Replacement Model serves to hold hospitals accountable for the quality and costs of care from time of surgery through 90 days after. “Bundling” payments in this way will incentivize hospitals and physicians to work together to provide the best quality care for patients both surgically and in time of recovery in order to reduce post-surgery complications.
The new system also rewards hospitals for quality care and quick recoveries with financial rewards, and penalizes subpar quality of treatment with requirements for hospitals to pay back Medicare a portion of the costs. This will further encourage increased coordination between acute care providers and Home Health Agencies, Skilled Nursing Facilities, and other Long Term Acute Care Hospitals in order to reduce complications or avoidable complications.
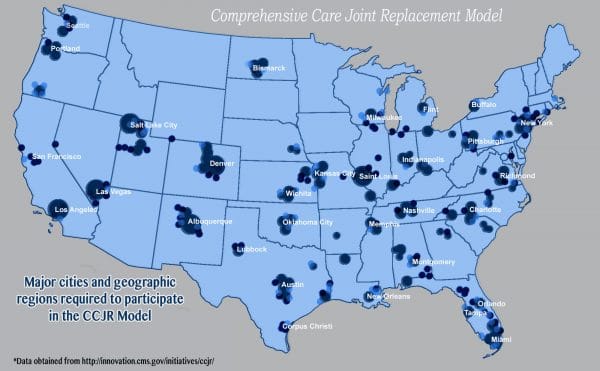
Under the new proposed method of payment, patients continue to choose their hospital, physician, long-term acute care provider, or other provider. The model is required in 75 metropolitan regions throughout the country and will bring in savings of $153 million over the next five years, according to CMS predictions.
It is among the first models that mandate participation from hospitals, and challenges may arise if hospitals lack the networks in place to accommodate for managing patients throughout the care episode. In anticipation of such difficulties, metropolitan areas with population more than 50,000 were chosen in an effort to include large urban hospitals chains, but certain smaller hospitals in the vicinity may face challenges. In addition, the responsibility of splitting and distributing bundled payment to the various providers in the continuum of care will fall to hospitals, serving as another potential challenge. Proposed areas of inclusion include New York, Denver, Orlando, Las Vegas, and Los Angeles, and Milwaukee (See map). All hospitals within these regions must participate unless already enrolled in another bundling pilot program.
Details regarding the model:
As defined by CMS, an episode consists of the admission of an Medicare-fee-for-service beneficiary to a hospital under the Inpatient Prospective Payment System (IPPS) and the discharge paid under MS-DRG 469(Major joint replacement or reattachment of lower extremity with Major Complications or Comorbidities (MCC)) or 470 (Major joint replacement or reattachment of lower extremity without MCC), as well as the subsequent 90 days including hospital care, post-acute care, and physician services.
Based on historical and regional pricing data, the CCJR sets target episode prices that will vary across participating hospitals in order to determine the “sweet spot” for future reimbursement. Adjustments are made with consideration to a variety of factors specific to the hospital, including the participant hospital’s average Hierarchical Condition Category (HCC) score, type of episodes initiated (MS-DRG 469 versus MS-DRG 470), variation in types of procedures, and patient-specific clinical indicators such as comorbidities.
At the end of each year, actual spending will be compared with the pre-determined CCJR target price, and hospitals are additionally rewarded or required to pay back depending on performance. Performance is determined by level of quality and cost efficiency as indicated by amount of complication, rate of readmission, and a patient experience survey.
The CCJM is a test demonstration that will last five years, beginning in January 2016. Hospitals and other providers will be paid under the usual Medicare FFS payment systems. During the first year, differences between actual episode cost and target price will not result in repayment or reward.
Bundling payments and assigning hospitals responsibility for the entire care episode aligns incentives for better coordination and efficiencies, promoting improved quality of care and patient outcomes. Conversely, it can potentially impose heavy financial strain on hospitals that lack extensive post-acute networks or experience managing patients post-discharge from the hospital.
Save
Save





